In recent years, experts around the world have noted an increase in degenerative-dystrophic processes in the ankle, gradually leading to disability. Arthrosis of the ankle joint often develops as a result of severe injuries or permanent microtraumas in athletes, professional dancers, circus performers. How to notice the signs of this disease in a timely manner and stop its progression, as well as how it is treated, you will learn from this article.
Arthrosis of the ankle - what is it
The ankle is a complex block-shaped joint formed by the lower (distal) ends of the tibia and fibula of the lower leg, forming the inner and outer ankles (ankles), as well as the talus of the foot. From the inside, it is strengthened by the deltoid ligament, from the outside - by the anterior and posterior talofibular and calcaneofibular ligaments. Function: flexion and extension of the foot. The ankle is functionally related to the foot, has common ligaments and muscle tendons with the joints of the foot.
Arthrosis of the ankle joint is a degenerative-dystrophic disease that begins with thinning and destruction of articular cartilage, reducing its depreciating properties, followed by the inclusion of all other articular tissues in the pathological process. The disease gradually leads to complete wear of the joint and disability. The code for osteoarthritis of the ankle joint ICD-10 is M19.
The disease is less common than a similar injury to the knee and is usually the result of severe injury or long-term injury from any activity.
The causes of osteoarthritis of the ankle
Specialists have studied in detail the reasons for the development of arthrosis of the ankle and arthrosis of the foot. This:
- injuries - intra-articular fractures of the joints, fractures of the ankles, complete and incomplete ruptures of ligaments and tendons;
- microtrauma due to any professional activity - these are ballerinas, dancers, professional athletes;
- increased load on the legs with excessive body weight;
- poor load distribution when wearing high-heeled shoes;
- metabolic disorders that have a negative effect on the metabolism of cartilage tissue - diabetes mellitus, obesity, gout, etc. ;
- hormonal changes, including age-related;
- transferred severe acute purulent arthritis;
- long-term chronic arthritis of any origin;
- osteochondrosis of the lumbar spine and intervertebral hernia, causing damage to the spinal roots and weakening of the leg and foot muscles, leading to joint instability and injury.
Mechanism of disease development (pathogenesis)
Under the influence of various reasons, blood circulation in the joint area is disturbed, which leads to a decrease in the volume of synovial fluid that supplies the cartilage tissue. Due to the lack of oxygen and nutrients, the cartilage becomes thinner, cracks and erosions appear on it. This leads to damage to the subcartilaginous layer of the bone. It thickens (sclerosing) and grows along the edges of the articular surfaces. These growths are called osteophytes. They compress soft tissues, blood vessels, and nerves, causing pain and further disrupting blood flow.
Due to circulatory disorders and high tension, the muscles suffer, they are weakened, which leads to joint instability and frequent dislocations. Arthrosis of the foot develops, small tarsal joints, metatarsotarsal, metatarsophalangeal and interphalangeal joints are affected.
Gradually, connective tissue grows in the joints, tightly binding the joint surfaces and disrupting joint function. Complete loss of ankle function is associated with fusion of bony joints. Foot osteoarthritis also develops gradually.
Symptoms of osteoarthritis of the ankle
Ankle osteoarthritis progresses slowly and imperceptibly at first. But the symptoms appear and gradually increase, signaling some kind of violation of the lower extremity.
First signs
The very first symptom of arthrosis of the ankle is pain during high loads, for example, during long walks, dances, football or volleyball matches, etc. This pain passes quickly, so the person does not immediately pay attention to it, attributing it to muscle fatigue. Pain can be both symmetrical in both joints (with high loads and microtraumas) and unilateral (after a major injury).
Then there is a feeling of stiffness in the morning or after a long stay in an immobile state. The ankles become stiff for a while, which makes movement difficult. At first it lasts a few minutes and passes after a slow pace. This symptom should already alert and become a reason for going to the doctor.
Overt symptoms
Gradually, the pain after exertion intensifies and lasts longer. The leg can hurt all day. Night pains join together, they usually appear in the second half of the night and are sometimes accompanied by painful muscle cramps. Periods of stiffness after immobility are also lengthened.
Due to severe pain, a person begins to limp when walking, tries to reduce pain in the foot by stretching or pressing it. Sometimes the ankle swells, the skin over it turns red, the pain intensifies. This is a sign of synovitis - inflammation of the inner synovial membrane. The inflammation is noninfectious in nature, develops from mechanical irritation, and resolves on its own without treatment. But at the same time, the exacerbation of synovitis activates the progression of the articular degenerative-dystrophic process.
Dangerous symptoms

Constant pain, aggravated by physical exertion, instability, loosening of the joint, a tendency to subluxations, dislocations and ligament damage are dangerous symptoms that require a visit to the doctor. The ankle changes externally: it takes on a different shape due to the invaded osteophytes. Osteoarthritis of the ankle (ankle) leads to its thickening. The movements of the foot are initially slightly limited, then the ankle becomes immobile or vice versa, loose, unstable. But even at this stage the patient can be helped, you just need to contact the clinic. Symptoms of arthrosis of the foot appear: pain in the foot, violation of its flexion and depreciation. The development of osteoarthritis of the big toe is accompanied by pain and deformity of the foot in the form of bulging and bending of the big toe outwards.
What is dangerous arthrosis of the ankle
The danger is that the disease first develops imperceptibly, and very often the patient goes to the doctor, already having an advanced stage.
Any localization and form of arthrosis leads to serious complications, so you should not delay treatment.
Classification
Ankle osteoarthritis can be primary, when the cause of its development is not established, and secondary, with a known root cause. Depending on the cause of development, the disease may have its own distinctive features.
Post-traumatic osteoarthritis of the ankle joint
The consequences of a traumatic injury are the most common cause of the disease. Post-traumatic arthrosis of the ankle joint can develop after a major injury - ligament rupture, dislocation, intra-articular fracture. Usually one joint is injured, so post-traumatic osteoarthritis is unilateral. A small, untreated wound may not be felt at first. And only after a while, when a person has already forgotten about it, a slight growing pain appears. This type of injury is dangerous because the patient comes to the doctor already in a neglected state. Serious injuries are treated better, their consequences appear faster, and the patient consults a doctor less late.
Discrete long-term microtrauma of both ankles is typical of professional dancers, athletes, and people whose professions are associated with long standing. There are symmetrical pains in the ankles during physical exertion. They are usually confused with muscle pain with fatigue, so it is also too late to consult a doctor.
Osteoarthritis of the ankle after osteoarthritis
The causes of these arthrosis can be chronic inflammatory processes of the joints (arthritis): rheumatoid, reactive, psoriatic. In this case, inflammatory processes are combined with degenerative-dystrophic (arthritis-arthritis). This speeds up the process of ankle destruction. With an exacerbation of inflammation, the joints swell, the skin over them turns red, the pain becomes very intense, especially at night. When inflammation decreases, metabolic disturbances predominate, while all processes develop very rapidly. The disease requires constant monitoring and treatment by a rheumatologist.
Much less often, the degenerative-dystrophic process develops after suffering from acute purulent arthritis. The purulent process destroys joint tissues, and after recovery, connective tissue forms in their place, which disrupts the function of the limb.
Arthrosis can also form after infectious arthritis - tuberculosis, gonorrhea, etc. The progression of the disease is associated with the main infectious process and the nature of the destruction. If the infection persists, joint destruction will progress.
Metabolic
Develops with a long gout course. Very often the first toe is affected. The other small joints of the foot and ankle are less commonly affected. Since gout attacks continue, it is difficult to determine outwardly when the degenerative-dystrophic process is occurring. You can only see it on an x-ray. In any case, the patient should be regularly observed by a rheumatologist and periodically examined.
Deforming osteoarthritis of the ankle joint
All types of osteoarthritis deform over time. Bone deformities indicate an advanced stage of the disease, when the cartilage has already collapsed, and the constant mechanical impact on the bone tissue contributes to its growth along the edges of the articular surface. This is how osteophytes are formed which change the joint shape.

Degrees of arthrosis of the ankle joint
There are several classifications, one of which distinguishes three clinical and radiological stages of osteoarthritis:
- Early. A little aches after standing or walking for a long time, some stiffness in the morning. All of this quickly disappears without any help. X-ray: normal or slight narrowing of the joint space.
- progressive. The pain after physical exertion is stronger and longer. Stiffness increases, a crunch appears in the joints during movement. Sometimes the joint swells, reddens and hurts a lot - a sign of synovitis. The X-ray shows a significant narrowing of the joint space, thickening of the subcartilaginous bone tissue (osteosclerosis) and proliferation of osteophytes.
- Final. The pain syndrome intensifies, becomes permanent. Because of the pain, a person limps, tucks his feet, uses a cane or crutches. The function of the limb is impaired, arthrosis of the foot and thumb develops. The complete absence of flexion-extensor movements is rare, usually against the background of arthrosis-arthritis. On X-ray: there is no joint space, osteosclerosis, large osteophytes deforming the joint.
Possible complications
If the disease is not treated and everything runs its course, the following complications are possible:
- persistent joint dysfunction and disability;
- intense and incessant pain in the ankle and feet, both after and without exertion;
- ankle instability with the development of habitual dislocations and subluxations;
- damage to the foot and thumb will join, which will further aggravate the patient's condition.
Diagnosis of osteoarthritis of the ankle
Before prescribing treatment, the doctor conducts an examination of the patient, which includes:
- medical interview and examination;
- additional research methods: laboratory tests (signs of inflammation and metabolic disorders are detected), instrumental studies (x-ray of the joint in two projections, magnetic and computed resonance imaging - early changes in bone structures and tissuesare detected), diagnostic arthroscopy (the internal articular surface is examined).
Treatment of osteoarthritis of the ankle joint
After making the final diagnosis, the doctor selects an individual treatment complex for the patient, consisting of drug and non-drug methods.
Medical treatment for osteoarthritis of the ankle
Medications are prescribed that have a symptomatic (eliminates the symptoms of the disease) and pathogenetic (suppresses the mechanism of disease development) effect.
Anti-inflammatories and analgesics
To eliminate pain, drugs from the group of nonsteroidal anti-inflammatory drugs (NSAIDs) are prescribed in short courses, they relieve pain and inflammation well (if synovitis has worsened):
- injection;
- rectal suppositories;
- oral tablets;
- skin patch.
Muscle relaxants
The muscles surrounding the diseased joint and performing its movement are in constant tension, which leads to their atrophy and increased pain. To eliminate muscle spasms, drugs from the group of muscle relaxants are prescribed.
Chondroprotectors
Medicines from the group of chondroprotectors contain glucosamine or chondroitin, and sometimes both of these substances. They protect cartilage cells from destruction and promote their restoration. They are prescribed in the form of injections, tablets and external agents (creams and ointments).
Preparations of hyaluronic acid for arthrosis of the ankle joint
To improve the damping abilities of synovial fluid and prevent further damage to cartilage and bone tissue, hyaluronic acid is injected into the joint cavity. This results in pain relief and better joint mobility.
Osteoarthritis gels and ointments for osteoarthritis of the ankle joint
External means can be used at home. Ointments for arthrosis of the ankle joint:
- NSAID gels are suitable for relieving pain and inflammation;
- to restore cartilage - gel and ointment based on chondroitin.
Non-drug therapy
The main methods of treating osteoarthritis of the ankle are non-drug. These are therapeutic exercises, massage, physiotherapy, wearing braces.
Physiotherapy
To alleviate the patient's condition and restore joint function, appoint:
- electrophoresis with medicinal substances;
- laser therapy;
- magnetic therapy;
- warming procedures - paraffin, ozocerite, in station conditions - mud applications.
Massage for osteoarthritis of the ankle joint
Massage courses improve blood circulation, which leads to the activation of metabolism, the restoration of articular and extra-articular tissues. The positive effect of massage on the muscles is the elimination of spasms, which contribute to the circulation of blood to the muscles, and the restoration of their strength, which is necessary to hold the limb in the desired position.
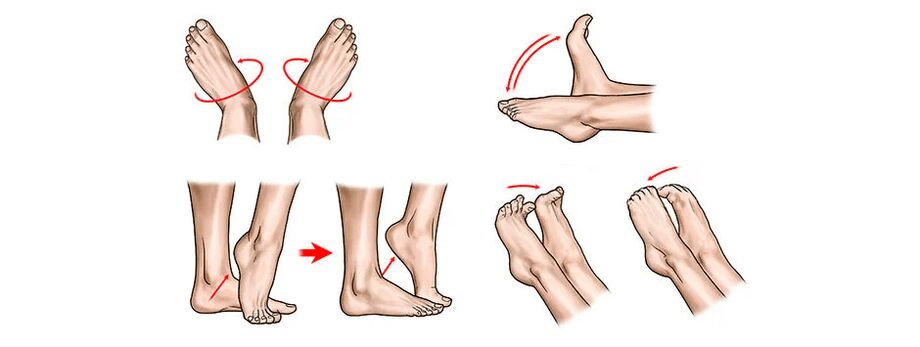
Exercises and exercise therapy for osteoarthritis of the ankle joint
Therapeutic gymnastics is a panacea for osteoarthritis. Motor activity is very important, in addition to exercise therapy, swimming is useful. The systematic implementation of the exercises selected by the doctor allows you to largely restore the function of the limb, even with advanced disease.
An approximate set of exercises (but before starting its implementation, you need to consult with your doctor):
Use of special orthopedic products
In order to prevent the progression of the disease, the doctor may prescribe the wearing of a special brace - a brace. It fixes the leg in the correct anatomical position, relieves muscle tension, improves blood circulation. Wearing an orthosis is prescribed by a doctor who also selects the most suitable model.
The fixation of the ankle can also be carried out using adhesive tape: With special adhesive tapes, the ankle is gently fixed in the desired position.

Surgical intervention
The operation is recommended for severe pain that is not eliminated by conservative treatment methods, as well as for significant dysfunctions of the limb.
Types of surgical procedures
The operations can be carried out in a traditional and gentle way:
- Therapeutic arthroscopy (sparing operations):
- sanitation of the joint cavity - with the help of an arthroscope, fragments of cartilage and bone tissue are removed from the cavity, which interfere with movement and cause pain;
- chondroplasty - the damaged cartilage layer is removed, which stimulates the growth of new cartilage cells (abrasive chondroplasty); in some cases, transplantation of sections of autocartilage taken from unloaded areas of the patient's knee joint (mosaic arthroplasty) is performed; chondroplasty is effective at the 2nd stage of the disease, when the joint has not yet lost its function.
- Arthrodesis is a classic surgical operation. It is carried out with a significant violation of the function of the limb, its looseness, habitual dislocations and pain. The joint is removed, the bones of the lower leg are fused with the bones of the foot. The ankle becomes immobile and serves only as a support.
- The endoprosthesis is the replacement of a worn and lost function of the ankle by an artificial function.
Features of rehabilitation after surgery
All operations are carried out in stationary conditions, after which experts recommend full rehabilitation. With sparing operations, rehabilitation is carried out on an outpatient basis with early inclusion during therapeutic exercises with the exception of high loads on the joint. After the stent, the patient stays in the hospital for a week, then rehabilitation measures are carried out on an outpatient basis. After two weeks, the stitches are removed and the patient can take a shower.
Diet food
There is no special diet for osteoarthritis. But to eliminate unnecessary stress on the ankle, it is necessary to maintain normal body weight. A person should receive proper and healthy nutrition, but the volume of high-calorie foods should be partially replaced with vegetables and fruits. Low-fat first and second courses, chicken, sea fish, cottage cheese, cheese, dairy products are useful.
traditional medicine
Using traditional medicine alone for osteoarthritis will not help. But they can be used as part of a complex treatment prescribed by a doctor. Here are some recipes:
- for oral administration: infusion of wild rosemary; Pour 20 g of finely chopped grass overnight in a thermos with 500 ml of boiling water, strain in the morning and take half a glass 4 times a day for a month; analgesic, restoration of cartilage tissue;
- for oral administration: take one mummy ball with a diameter of 0. 5 cm in the morning, chewing well, 30 minutes before meals for 10 days; interrupt 5 days, then repeat everything 3 more times; excellent stimulator of metabolic processes;
- honey massage: apply lukewarm liquid honey to the ankle before going to bed and rub lightly, massaging the tissues, for 5 minutes; then wrap the leg in a warm shawl and leave until morning; restores blood circulation and metabolism in the cartilage tissue.
Approach to treatment in clinics
Clinic doctors have developed their own approach to the treatment of diseases such as arthrosis of the ankle and foot. At the initial appointment, a thorough examination of the patient is carried out, the doctor carefully listens to his complaints and the history of the disease, after which he prescribes additional laboratory and instrumental studies, including MRI. Only after this the doctor makes the final diagnosis, prescribes and agrees with the patient on complex treatment. That consists of:
- modern schemes of drug and non-drug treatment of arthrosis - drugs, physiotherapy, exercise therapy and massage, methods of fixing the ankle;
- traditional methods of oriental therapy - acupuncture, moxibustion, acupressure, various methods of physiotherapy, including taping.
These are not all the methods used in clinics. Doctors are able to combine Western and Eastern methods, significantly accelerating the improvement of the patient's condition. Patients quickly get rid of pain, their quality of life improves significantly.
Combination of proven techniques from the Orient and innovative methods from Western medicine.
Prevention of osteoarthritis of the foot
To reduce the risk of disease progression, the following recommendations should be followed:
- activity, exercise therapy exercises, swimming should be part of your life;
- high physical activity and any traumatic factors should be excluded; hiking should be combined with rest, if the legs are injured during work, it is worth changing it;
- injuries, especially in winter on ice, should be excluded by thinking about the means of movement and shoes used;
- rational nutrition is necessary to restore metabolism, but being overweight is an additional load on the ankle, get rid of it;
- preventive cures are the guarantee of a pain-free life.
Frequently asked questions about the disease
- Which doctor should I contact for osteoarthritis of the ankle and osteoarthritis of the foot?
To the orthopedist-traumatologist. But if the disease developed against the background of some kind of rheumatic process, then to a rheumatologist.
- What predictions do doctors usually give?
It is possible to stop the progression of the degenerative process and improve the quality of life at any stage, but it is better to do this at the onset of the disease, do not wait for the appearance of complications.
- Can ankle osteoarthritis develop in children?
Perhaps after an injury or against the background of congenital pathology.
- What are the consequences of the disease?
Untreated osteoarthritis leads to disability. If you start treatment in time, it is quite possible to preserve the function of the limb. Treatment at later stages will relieve pain and improve quality of life.
- Are sports injuries a cause of ankle osteoarthritis?
Yes, sports injuries are one of the main causes of this disease.
- Is it possible to make scotch ankle with arthrosis?
It is possible, but it must be done by a specialist.
Osteoarthritis of the ankle joint is almost always the result of macro or microtrauma. It proceeds slowly and imperceptibly at first. Therefore, timely treatment and rehabilitation after injury is so important, as well as contacting a doctor at the first signs of ankle disease.































